In vitro fertilization (IVF) is an assisted reproduction technique that has transformed the lives of millions of couples around the world. Since its introduction in 1978 with the birth of Louise Brown, the first "test tube baby", IVF has advanced considerably, offering solutions to infertility problems previously considered insurmountable.
History of In Vitro Fertilization
The development of in vitro fertilization dates back to the pioneering work of several scientists throughout the 20th century. However, the most significant breakthrough occurred in 1978 when Robert Edwards and Patrick Steptoe achieved the first successful birth through IVF. This milestone marked the beginning of a new era in reproductive medicine, providing hope to couples struggling with infertility.
Since then, IVF has evolved with technological and scientific improvements that have increased success rates and reduced associated risks. Innovations such as intracytoplasmic sperm injection (ICSI), preimplantation genetic diagnosis (PGD), and embryo freezing have allowed IVF to become a viable option for a greater number of people.
The Process of In Vitro Fertilization
The IVF process can be divided into several fundamental stages:
1. Ovarian Stimulation
The first step in IVF is ovarian stimulation. This process involves the use of hormonal medications to stimulate a woman's ovaries, with the goal of producing multiple mature eggs instead of just one. These medications are usually gonadotropins, which are administered by daily injections for approximately 10-14 days. During this period, ultrasounds and blood tests are performed to monitor the growth of the follicles and adjust the dose of medication if necessary.
2. Egg Retrieval
Once the follicles have reached the appropriate size, an injection of hCG (human chorionic gonadotropin) is scheduled to induce the final maturation of the eggs. Approximately 36 hours later, egg retrieval is performed using ultrasound-guided follicular aspiration. This procedure is performed under sedation or light anesthesia and lasts between 20 and 30 minutes.
3. Fertilization
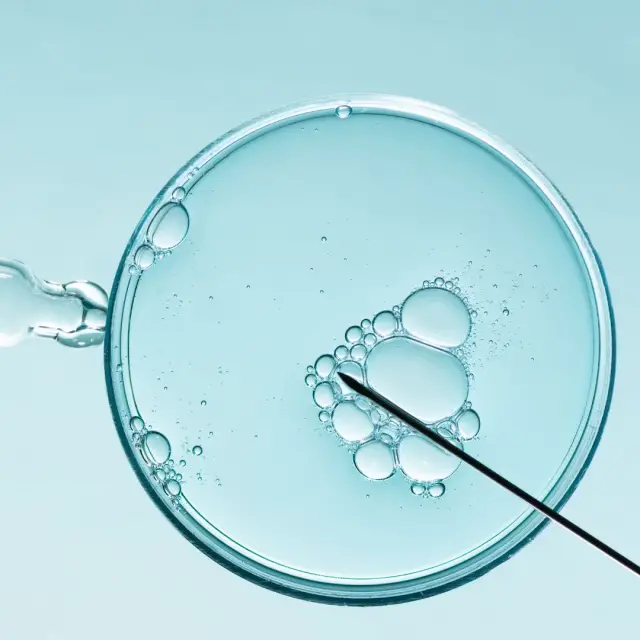
The recovered eggs are mixed with the partner's or a donor's sperm in a specialized laboratory. Fertilization can occur naturally in a culture dish (conventional IVF) or through ICSI, where a single sperm is injected directly into the egg. The choice of method depends on factors such as sperm quality and the couple's fertility history.
4. Embryo Culture
The resulting embryos are grown in a special medium in the laboratory for 3 to 5 days. During this time, embryologists monitor the development of the embryos, evaluating their quality and viability. In some cases, preimplantation genetic diagnosis (PGD) can be performed to detect genetic abnormalities before transfer.
5. Embryo Transfer
Once the embryos have reached the appropriate stage, one or more are selected to be transferred to the woman's uterus. This procedure is relatively simple and does not require anesthesia. Using a thin catheter, the embryos are carefully deposited into the uterine lining. The remaining good quality embryos can be frozen for future use.
6. Pregnancy Test
Approximately 10-14 days after the embryo transfer, a pregnancy test is performed using a blood test to determine if the procedure has been successful. If the test is positive, ultrasounds are scheduled to confirm the viability of the pregnancy and monitor its progress.
Applications and Benefits of In Vitro Fertilization
IVF is used to treat a wide variety of infertility problems, including:
Tubal factor infertility: Blockage or damage to the fallopian tubes that prevents the union of the egg and sperm.
Male infertility: Problems with the quantity or quality of sperm.
Endometriosis: A condition in which tissue similar to the lining of the uterus grows outside of it, affecting ovarian and tubal function.
Unexplained infertility: When a specific cause of infertility cannot be identified.
Ovulatory problems: Disorders that affect the release of eggs from the ovaries.
Fertility preservation: For women who want to delay childbearing or who are going to undergo treatments that may affect their fertility, such as chemotherapy.
Advantages of IVF
High success rate: IVF offers a high probability of pregnancy, especially in women under 35 years of age.
Control over the reproductive process: Allows couples and single women to have greater control over the timing and conditions of conception.
Fertility Preservation: Freezing eggs and embryos provides an option to maintain future fertility.
Genetic diagnosis: PGD allows the detection of genetic diseases before implantation, reducing the risk of transmitting hereditary disorders.
Disadvantages and Risks of IVF
Despite its numerous benefits, IVF also has disadvantages and risks that must be considered:
High cost : IVF is an expensive procedure, and may require multiple cycles to achieve a successful pregnancy.
Medication side effects: Hormonal medications can cause side effects such as bloating, nausea, and mood changes.
Risk of multiple pregnancies : Transferring multiple embryos increases the risk of twins, triplets, or more, which can complicate the pregnancy.
Medical complications: Although rare, complications such as ovarian hyperstimulation syndrome (OHSS) and infections can occur.
Social and Ethical Impact of In Vitro Fertilization
IVF has had a significant impact on society and has raised several ethical questions. As technology advances, new considerations arise about its use and implications.
Ethical Issues
Some of the most prominent ethical issues include:
Embryo selection: The possibility of selecting embryos based on genetic characteristics raises questions about eugenics and the acceptance of genetic diversity.
Destination of surplus embryos : The freezing and eventual discarding of embryos raises dilemmas about the moral and legal status of the embryos.
Access and equity: The high cost of IVF may limit its accessibility, raising questions about justice and equity in access to fertility treatments.
Social impact
IVF has changed the perception of infertility and reproduction, offering new opportunities and challenges:
Changes in family structure: IVF has allowed same-sex couples, single women and older couples to form families, challenging traditional family norms.
Reducing stigma: By offering a viable solution to infertility, IVF has helped reduce the stigma associated with this condition.
Legal Considerations: The need for regulation and legislation around IVF has led to debates and policies regarding reproductive rights and the protection of those involved in the process.
Finally, the future of IVF promises continued advances that will further improve its effectiveness and accessibility. Some areas of development include:
Gene Editing Technology
CRISPR technology and other gene editing techniques have the potential to eliminate inherited diseases before implantation. However, its use in assisted reproduction raises important ethical questions and requires careful regulation.
Artificial Intelligence and Big Data
AI and big data analytics can improve embryo selection, optimize treatment protocols, and personalize healthcare to increase IVF success rates.
Advanced Laboratory Techniques
Improvements in embryo culture techniques, vitrification (ultra-rapid freezing), and embryo biopsy promise to increase implantation rates and reduce associated risks.
Global Accessibility
Efforts to reduce the costs and increase the accessibility of IVF in developing countries can democratize access to this technology, allowing more people to benefit from its advances.
In vitro fertilization has revolutionized reproductive medicine, providing hope and solutions to millions of people struggling with infertility.